Stem cell technology has produced some very exciting advances in medicine recently. Now a recent study from Penn State details how researchers coaxed ordinary skin cells to grow into heart cells.
Because experimenting with embryonic stem cells comes with ethical problems, researchers have learned how to induce skin cells to differentiate into other cells the way stem cells do. Researchers at Penn State were able to use induced pluripotent stem cells, as they’re called, to become epicardium cells—those that cover the outer layer of the human heart. Their results were published in the journal Nature Biomedical Engineering.
Xiaojun Lance Lian, lead author and assistant professor of biomedical engineering and biology at Penn State, primarily focuses on human stem cells to treat human disease. “We decided to study heart disease. It’s caused by the death of heart muscle cells, which then destroy the heart wall. So we are trying to repair the human heart wall in the lab and later on transplant this tissue into the patient,” Lian tells mental_floss.
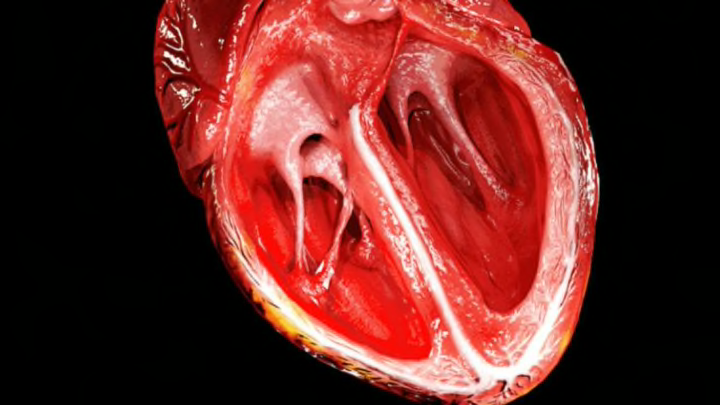
In 2012, his team started working on stem cell differentiation to make heart cells, with the aim of one day using them to treat heart disease and its related conditions, like heart attacks. Lian explains that the heart wall is comprised of “three layers, just like a sandwich.” The inner layer is the endocardium, the outer layer is the epicardium, and between them is the muscle layer known as the myocardium.
As of 2012, Lian could create myocardium cells using human “progenitor” stem cells—provided by Swedish company AstraZeneca—but wasn’t able to get the cells to differentiate into the outer layer of epicardium cells. In order to do that, Lian and his team needed to determine a new signaling pathway to nudge the cells into differentiation. They looked to the Wnt signaling pathway, composed of proteins that send signals into a cell using its cell-surface receptors—causing the cells to become the outer layer cells instead of the muscle layer.
Not only were they successful, Lian says, “we did a comparison between our cells and the real human cells, and found they were very much like each other.”
Another exciting breakthrough came when the team learned to create reporter cells, which have had their marker genes tagged with green fluorescent protein. When they showed up in the petri dish, their green glow would give them away from other cell types. The scientists tested numerous molecules before they successfully turned them fluorescent, which Lian calls “the most exciting moment” of the research.
Equally as exciting to him was the discovery of a way to keep cells proliferating. Typically, adult cells that are cultured in the lab will stop proliferating after 10 days. But Lian discovered that applying the cell-signaling pathway known as transforming growth factor beta (TGF-β) to the media the cells were growing in encouraged the cells to continue proliferation beyond 50 days.
“Say you want to generate 10 billion cells for a clinical trial,” Lian explains. “You would need to start from the very beginning with the stem cells and differentiation … But if the cells keep proliferating, you use the cells you have and just culture them to make as many cells as you want,” which is a huge advantage, he notes.
Together, these advances bode well for clinical applications of stem cell therapy after heart attacks. Heart attacks usually occur due to blocked blood vessels, which starve the heart muscle of nutrients and oxygen, and eventually kill heart muscle cells. When this occurs, “the heart won’t function properly,” Lian says.
But animal studies suggest that “if you transplant the outer layer of epicardium cells in that damaged region, these cells could further differentiate into the cells there. They could provide the vessels there—the supporting matrix. They could also potentially become the cardiac muscle.” Of course, further research is needed, and Lian’s lab plans to conduct larger animal studies on rabbits, pigs, and non-human primates next. If those trials prove successful, they aim to move to human trials. Lian is hopeful that one day scientists may even be able to regenerate an entire heart wall.