Bad news for good cholesterol: A Danish study published in European Heart Journal finds that people with extremely high high-density lipoprotein (HDL, often called “good” cholesterol) levels face a higher, not lower, risk of death.
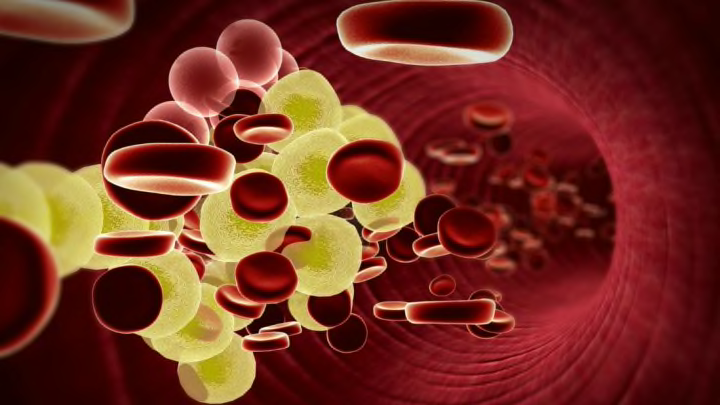
Cholesterol as a substance is neither good nor bad, but an important part of our body chemistry. Like most things, in moderation, it's fine; the health risks set in once our levels get out of whack. Scientists and doctors have long understood cholesterol as a sort of angel-on-one-shoulder, devil-on-the-other situation, in which low-density lipoprotein (LDL) is harmful and HDL is helpful. HDL mediates LDL's negative effects, which means that having more HDL is good.
Or at least that's what we thought.
Researchers pulled health information on 116,000 people from the Copenhagen City Heart Study and the Copenhagen General Population Study, then cross-checked it against death reports from the Danish Civil Registration System. They followed study subjects for six years, during which more than 10,500 people died.
What they found surprised them. Extremely high levels of HDL were associated with significantly greater risks of death than normal levels—68 percent higher for women and a staggering 106 percent for men. Men with very high HDL (one step down from "extremely high") were 36 percent more likely to die.
"These results radically change the way we understand 'good' cholesterol. Doctors like myself have been used to congratulating patients who had a very high level of HDL in their blood. But we should no longer do so, as this study shows a dramatically higher mortality rate," co-author Børge Nordestgaard of the University of Copenhagen said in a statement.
Before we get too worried, it's worth noting that these extremely high HDL levels were incredibly rare, affecting only 0.4 percent of male participants and 0.3 percent of women. The researchers say these people were also more likely to share unusual genetic variants. It's possible that these genes and not the cholesterol are responsible for their higher mortality rates.
Some elements of our ideas about cholesterol still held true. People with extremely low HDL levels also faced an increased mortality risk.
The safest levels seemed to be right in the middle, at 1.9 mmol/L for men and 2.4 mmol/L for women.
More research is needed, as this study focused exclusively on white Danish people and only looked at correlation, not causation.
Still, Nordestgaard said, "It appears that we need to remove the focus from HDL as an important health indicator in research, at hospitals and at the general practitioner. These are the smallest lipoproteins in the blood, and perhaps we ought to examine some of the larger ones instead."