We tend to think of our brains as one big organ inside our skulls, but it’s actually comprised of many, small structures that make it possible for us to walk, talk, think, and feel. Of these, one of the more well-known structures, the amygdala, has been found to play a hugely important role in many social and emotional processes—influencing everything from health to addiction.
Mental_floss spoke to Rahul Jandial, a neurosurgeon and neuroscientist at City of Hope Cancer Center in Los Angeles, California, and Brandon Brock, a staff clinician at the Cerebrum Health Centers Brain Initiative Group in Texas, about this fascinating part of the brain.
1. IT'S NOT REALLY ONE STRUCTURE …
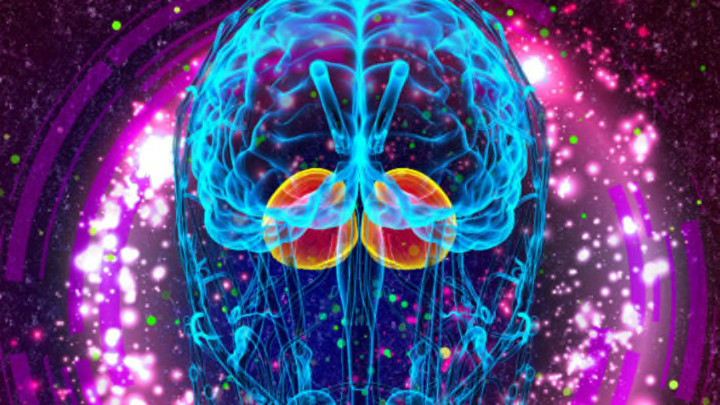
One of the more well-known structures, the amygdala is located within the depths of the anterior-inferior temporal lobe. The almond-shaped region is part of the limbic system and is actually a paired structure, with parts in each temporal lobe, according to Jandial.
He says you can survive with only one of the two: “How do I know? I can surgically remove one as part of a brain surgery called selective amygdalohippocampectomy.” In fact, in studies where rats, monkeys, or rabbits have their amygdala removed, the animals live normal lives except for one notable new development: They don’t feel fear.
2. … BECAUSE THE AMYGDALA IS YOUR BRAIN'S FEAR FACTORY.
Your fear of snakes and scary movies is in large part due to the function of your amygdala, which “responds before frontal lobes weigh in,” Jandial says. It’s part of your instinctive brain and serves as your “emotional thermostat.” He adds, “It’s not in charge of just fear, but all deep and visceral emotions—one of those ancient brain regions that can defy the frontal lobe request.”
According to a 2007 study in Social Cognitive and Affective Neuroscience, “amygdala activity may represent the generation of emotional experience itself, and/or it may reflect sundry aspects of emotional information processing correlated with emotional experience.”
3. THE AMYGDALA ALSO HAS A TRUE MIND-BODY CONNECTION.
And yet the amygdala has purposes beyond fear. It has been shown to assist in emotional learning, “whereby cues acquire significance through association with rewarding or aversive events,” according to a paper in Current Opinion Neurobiology. More recent research, the authors write, suggest that the amygdala regulates additional cognitive processes, such as memory or attention.
With its ability to interpret sensory stimuli in the world and translate them into physical reactions, the amygdala, as a research paper in Social Cognitive and Affective Neuroscience suggests, “may thus represent embodied attention—the crucial link between central (mental) and peripheral (bodily) resources.”
4. DAMAGE TO THE AMYGDALA CAN LEAVE YOU HORNY AND HUNGRY.
An injured amygdala can leave a person “super hungry, sexually aroused, and fixated with putting things in their mouth,” says Jandial. In other cases, it can lead to a reduced fear of risks, and thus an increase in risky behavior. Researchers found that adult monkeys who were given amygdalectomies “showed more pro-social cues and less avoidance behaviors toward other (healthy) monkeys.” In one extreme case, damage to the amygdala shut down one woman’s ability to feel fear altogether.
5. IT ALSO PLAYS A ROLE IN PAIN.
Fibromyalgia is a disease characterized by "widespread musculoskeletal pain with diffuse tenderness at multiple tender points,” as a study in Clinical Neuroscience describes. Brock says that changes in the amygdala’s volume and function play a role in both fibromyalgia and chronic pain syndromes. This appears to be a consequence of the amygdala becoming hypervigilant and oversensitized to internal sensations of pain or trauma, according to a study in Explore. “This results in exhaustion of the neuro-endocrine and immune systems and chronic physical and mental exhaustion, as well as many secondary symptoms and ongoing complications.”
6. THE AMYGDALA IS KEY TO UNDERSTANDING ADDICTION.
Addiction is considered a brain disease by the medical community rather than a lack of willpower or a character defect. According to a study in Brain Research, a common addiction cycle comprises three stages—“preoccupation/anticipation, binge/intoxication, and withdrawal/negative affect—in which impulsivity often dominates at the early stages and compulsivity dominates at terminal stages.” The amygdala becomes recruited in the final withdrawal stage, where it sends stress signals to the body, driving a person to crave more of their substance.
7. DESPITE ADVANCES IN BRAIN-IMAGING TECHNOLOGY, IT'S STILL DIFFICULT TO STUDY.
Though we know much more about the amygdala since it was first discovered in the 1930s in monkeys, there’s still much to learn. Because of the amygdala’s deep brain location and its entanglement with other neighboring brain structures, it’s difficult to find “exact ways to monitor its function, output and all regions that it has a synaptic influence on. Time and further scientific research will hopefully unveil that,” Brock explains.