The humble ankle has had a remarkable history as an object of fetishization: Think Victorian sexual repression and high heels. Of course, its significance is also practical. Without ankles, there would be no sports or dance. Not only would nobody be able to score a touchdown, we wouldn't even be able to walk. Here are eight things you may not have known about this basic but crucial joint:
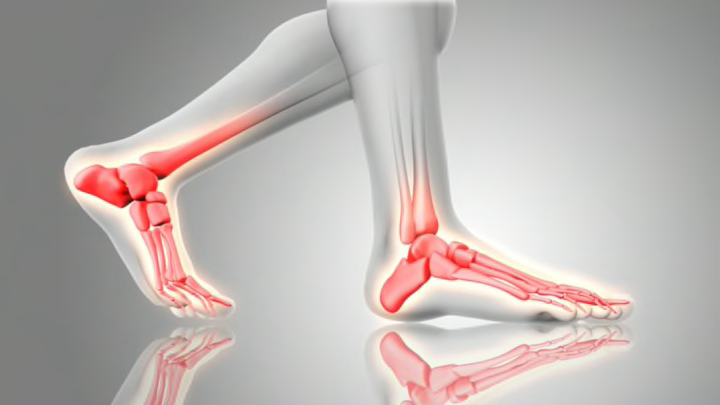
1. THE ANKLE IS COMPOSED OF JUST THREE MAIN BONES.
The true ankle joint is composed of three bones: the tibia, or the inside part of the ankle; the fibula, the outside part of the ankle, and the talus, underneath. These allow the flexion and extension of the foot, letting you make the up and down motions that you require to walk. Below the ankle joint is actually a second joint called the subtalar joint, which allows side-to-side motion of the foot. Altogether, the human foot and ankle contain 26 bones, 33 joints, and more than 100 muscles, tendons, and ligaments.
2. THE ANKLE JOINT IS NOTORIOUSLY WOBBLY.
Despite how often humans are on their feet, the ankle joint is small and unstable in the best of times because of its precarious anatomical structure. Most people will experience a tweaked, twisted or sprained ankle at least once in their lives.
3. ANKLE SPRAINS ARE THE MOST COMMON INJURY IN AMERICA.
When you couple the weak ankle joint with the vigorous activity it’s required to perform, it’s no surprise that ankle sprains account for nearly 2 million injuries every year, or 20 percent of all sports injuries in the United States.
4. NOT ALL OF THESE SPRAINS ARE SPORTS-RELATED.
Researchers from the University of Alabama at Birmingham reported an estimated 125,355 high heel-related injuries in U.S. Emergency Departments between 2002 and 2012. In 2011 alone, there were a reported 19,000 injuries from high heels. The injury rate was greatest for women in their 20s. Another survey from the College of Podiatry found that most women reported foot pain after one hour and six minutes of wearing high heels, and 20 percent of participants said that they felt pain after just 10 minutes of wear.
5. NEVER JUST "WALK OFF" AN ANKLE SPRAIN.
You can actually do significant damage if you’re walking on an untreated ankle sprain, according to the National Athletic Trainers’ Association. Treatments may range from rest, ice, and ibuprofen to casts, braces, and even surgery. Always seek a doctor’s care if you think you’ve sprained an ankle.
6. THE ANKLE WAS TOO EROTIC FOR PUBLIC VIEWING IN VICTORIAN ENGLAND.
A woman lifting her skirt to show her ankle was considered provocative in Victorian England. This is ironic, given that the Victorians were at the same time producers of copious pornography.
7. "PRETTIEST ANKLE" CONTESTS WERE POPULAR THROUGH THE 1930s.
While the Victorian era repressed women’s displays of their bodies, the 1930s were all about exposing the ankles. In fact, according to Mashable, in the UK “pretty ankle” competitions were popular events until about World War II.
8. YOU MIGHT WANT TO RETHINK AN ANKLE TATTOO.
Because the foot and ankle generally don’t have much fat or flesh, getting a tattoo on this skinny extremity can be extremely painful. Because of how much use your foot and ankle get, they also can take twice as much time to heal as other locations—but it could give you a leg up in an ankle competition.