Scientists Make Antibiotics from Bacteria Found in the Human Body
We’ve all got hidden potential within us. Some of it is apparently hidden very, very deep: scientists have used bacteria found in the human body to create two powerful new antibiotics. They described their work in the journal Nature Chemical Biology.
The search for new antibiotics has become something of an arms race between researchers and the bacteria they’re trying to kill. The more antibiotics we use, the faster bacteria become resistant to our drugs, and the more pernicious their infections become. If we don’t come up with some new solutions soon, we’ll be facing a world awash with dangerous superbugs and no cures.
So drug researchers at The Rockefeller University have started thinking outside the box. Rather than building new pharmaceuticals from the ground up, they’ve been looking for them, well, in the ground, investigating natural materials like soil and sand in the hopes of finding a new bacteria-slaying tool.
One team of researchers at the university has set their sights ever so slightly higher, tapping not only the dirt but the bacteria-covered organisms that walk it. And by organisms, we mean people. Our bodies are crawling with bacteria, inside and out. Who knows what those little critters can do?
To find out, scientists from the Laboratory of Genetically Encoded Small Molecules decided to conduct a thorough search of the human microbiome (the collective term for the microscopic ecosystems sharing our bodies). They tapped into public microbiome databases, searching for gene clusters that could make molecules called non-ribosomal peptides (NRPs). NRPs have a lot of different skills. Some produce toxins, while others produce pigment. Others kill bacteria.
The search yielded 30 different NRP-making gene clusters, which the team then recreated in the lab. They set their newly grown clusters to work and coaxed them into producing 25 different chemical compounds. The team then pitted those compounds against various human pathogens to see if any could win. Two compounds, both derived from microbes in the genus Rhodococcus, succeeded. The researchers dubbed these new antibiotic contenders humimycins (from “human,” “microbiome,” and “mycin,” a common suffix for antibiotics).
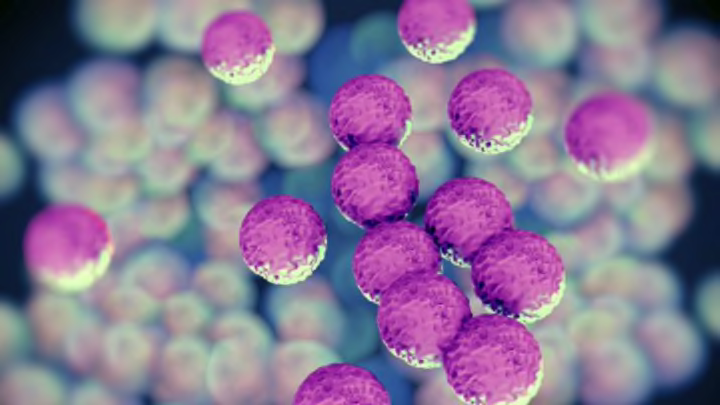
The new humimycins were especially tough on Staphylococcus and Streptococcus bacteria (commonly known as staph and strep)—two pathogens known for overcoming and growing resistant to other drugs. Not only did the humimycins work on their own, but they also proved to be pretty good at breaking down the bacteria’s drug resistance so that other antibiotics could get in there and finish them off.
Combining these new compounds with existing drugs could be the secret to shutting infection down, lead researcher Sean Brady said in a statement. “It’s like taking a hose and pinching it in two spots," he said. Even if neither kink can stop the flow of water on its own, “eventually, no more water comes through.”