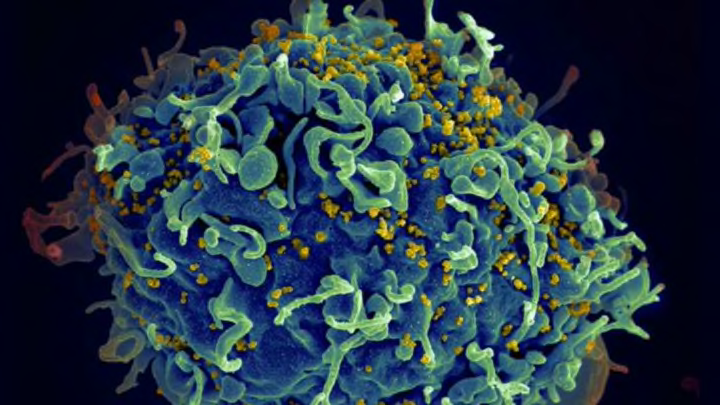
A human T cell (blue) under attack by HIV (yellow), the virus that causes AIDS. The virus specifically targets T cells, which play a critical role in the body's immune response against invaders like bacteria and viruses. Image credit: Seth Pincus, Elizabeth Fischer and Austin Athman, National Institute of Allergy and Infectious Diseases, National Institutes of Health
The global spread of AIDS was one of the greatest public health crises of the last century. While we’ve made tremendous advances in human immunodeficiency virus (HIV) prevention and treatment, the details of the virus’s global spread have been harder to pin down. A new report published this week in Nature sheds light on when and where HIV arrived in the United States: in New York City around 1970. It also removes blame from the man long known as "Patient Zero"—he was not, in fact, the first person in North America to contract the virus.
Because HIV attacks the immune system, limiting the body's ability to fight infections or infection-related cancers, the first patients presented with a range of symptoms, from enlarged lymph nodes and pneumonia to cancer. Physicians in California first recognized it as a single entity in 1981, but the disease didn’t get a name—acquired immunodeficiency syndrome (AIDS)—until a year later. By then, media reports of a “gay cancer” had begun to raise alarms and stigma across the country. The first drugs to treat HIV were not approved until 1987, by which time the disease had taken more than 40,000 lives.
Part of the problem lay in the limitations of medical and scientific technology. We didn’t have the capability to look inside the disease with the level of detail required to stop it. Blood tests could pick up on the presence of HIV in a sample, but they couldn’t spell out its genetic code. To do that, said study co-author and virus evolution expert Michael Worobey of the University of Arizona, researchers would need a sample of RNA from the virus itself—a serious challenge, as the virus’s RNA is super delicate and breaks down at the slightest provocation.
But we’ve come a long way since then. Worobey and his colleagues in Arizona and at the University of Cambridge have created a vividly named new technique called RNA jackhammering that allows them to break down the human genes in a blood sample and extract and examine the virus RNA hiding within them.
To rewind the clock to HIV’s early days in the States, the researchers applied their jackhammers to blood samples taken from more than 2000 men in New York and San Francisco in 1978 and 1979. The nearly 40-year-old samples had degraded since their collection, but Worobey and his colleagues were still able to extract eight near-complete HIV RNA sequences, creating the oldest-known record of North American HIV genetics.
By comparing these sequences with those collected from other parts of the globe, the researchers were able to trace the virus’s evolution and devastating spread. They found that HIV had crossed from Africa to the Caribbean, and from there jumped to New York City and then San Francisco, where the first patients were identified. These findings run counter to earlier theories, which pinpointed the virus’s U.S. landfall to San Francisco.
The density of vulnerable populations in New York City were like “dry tinder” for HIV, Worobey said in a press statement, "causing the epidemic to burn hotter and faster and infecting enough people that it grabs the world's attention for the first time.”
By the time the blood samples were collected, the authors say, the virus had already evolved into the form it bears today.
Their analysis also upends another well-known element of the AIDS story: the identity of “Patient Zero.” For nearly three decades, scientists have traced the virus’s entry to the U.S. back to one man: Gaëtan Dugas. But Worobey and his colleagues tested a sample of Dugas's blood from 1983 and found that the virus RNA in his blood was no less evolved—and therefore no older—than the viral genes in his peers. He wasn't Patient Zero.
That the weight of the AIDS pandemic ever came to be placed on Dugas's shoulders at all may itself have been a simple typographical error, the authors write. The man’s original file identified him as a patient from Outside of California, or Patient O. Somewhere along the way, the letter O became a zero, a mistake that would be perpetuated for decades—long after Dugas himself had died.
The authors are hopeful that their findings and their new technique will help accelerate scientific unraveling of the virus.
"Earlier detection and better alignment of the various options we have to make it harder for the virus to move from one person to the next," Worobey said, "are key to driving HIV out of business."
Know of something you think we should cover? Email us at tips@mentalfloss.com.