One symptom of Parkinson’s disease is involuntary hand tremors that make simple tasks like getting dressed or eating breakfast a daily struggle. After being assigned to care for a Parkinson’s patient as a medical student when he was 24, Faii Ong was inspired to devise an innovative new treatment for the disease.
Ong’s GyroGlove uses some clever physics borrowed from childhood toys to calm hand tremors in patients with the condition. “Mechanical gyroscopes are like spinning tops: they always try to stay upright by conserving angular momentum,” Ong, now 26, explained to MIT Technology Review. “My idea was to use gyroscopes to instantaneously and proportionally resist a person’s hand movement, thereby dampening any tremors in the wearer’s hand.”
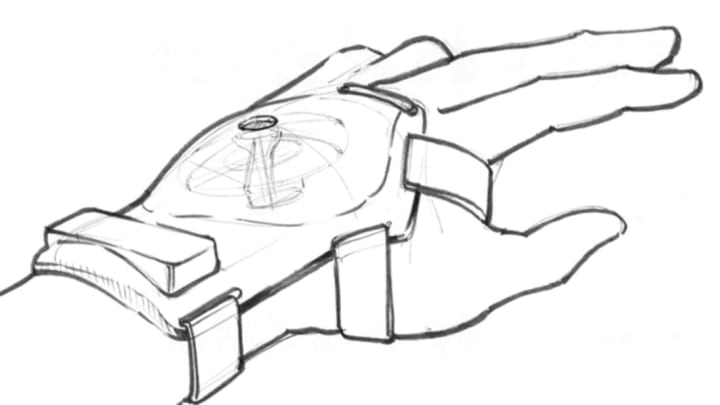
Working with a team of fellow students from Imperial College London, Ong developed a prototype of the glove outfitted with a miniature, dynamically adjustable gyroscope on the back of the hand. The effect it produces is similar to the sensation of moving your hand through heavy molasses: movement is hampered without being prevented entirely. In early tests, the battery-powered gyroscope was shown to reduce hand tremors by up to 90 percent.
Adjustments still need to be made to the technology before the GyroGlove is ready for commercial production, but the team’s mentor, Imperial College professor of musculoskeletal biodynamics Alison McGregor, told MIT Technology Review that the device “holds great promise and could have a significant impact on users’ quality of life.”
The device has potential applications beyond Parkinson’s treatment as well; Ong says he could see the glove being used in professional fields such as surgery or photography where a steady hand is essential. A precise cost and launch date for the product have not yet been revealed, but the team says they're aiming for a UK launch sometime before September at a price between about $550 to $850 USD.
[h/t: MIT Technology Review]