Scientists have long looked to anatomy and neurology to understand and ameliorate stress responses in humans. Now, a pioneering study, recently published in Proceedings of the National Academy of Sciences, suggests that mitochondria—the tiny energy centers inside our cells, which convert food into ATP, the crucial molecule that stores the energy humans need to do pretty much everything—may play a more significant role in the stress responses of mammals than previously understood, and even in understanding psychiatric and neurologic diseases.
The study was headed by Douglas Wallace, director of the Center for Mitochondrial and Epigenomic Medicine at The Children’s Hospital of Philadelphia and a leading researcher in the genetics of mitochondria for 40 years. He is among the first to prove that defects in energy metabolism can cause disease.
Wallace and his team found that even slight changes in mitochondrial genes had a large effect on how mammals respond to stress in their environments. Wallace’s team bred mice with different genetic mutations to their mitochondrial DNA (mtDNA). “With these mutants in hand we could expose them to a mild environmental stress, such as 30 minutes in confinement,” Wallace tells mental_floss.
They then measured the neuroendocrine, inflammatory, metabolic, and gene transcription systems, which are the systems most effected by stress. “We found the changes in mitochondrian response had a markedly different response from normal mitochondria,” he says.
They mixed two normal, but different, mtDNAs in mice to prevent maternal inheritance of the mtDNA. This resulted in “hyperexcitable mice with severe learning and memory defects,” according to a press statement.
Because humans and mice share a similar degree of variation in their mtDNA, Wallace suspects that the mouse results “might have a comparable effect” in human DNA.
While research is conflicting about how much stress increases risk of disease, psychiatrists have a term for the common physiological decline that happens when people are under continuous stress: allostatic load. “What is the connection between stress and declining bodily functions?" Wallace says. "The intermediate is the mitochondria.”
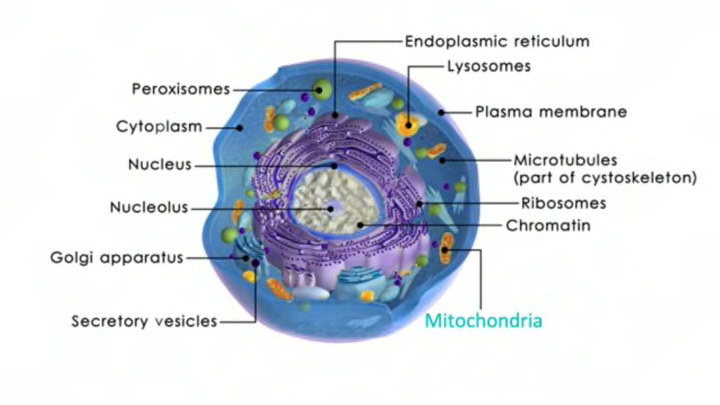
Wallace believes that the bioenergetics of mitochondrial function is the overlooked piece in understanding everything from psychiatric and neurologic diseases to aging, partly a result of the current “anatomical paradigm” in the scientific community, which focuses mostly on nuclear DNA, anatomy, and neurology. “What’s missed is the realization that mitochondria is much more important than just making ATP," he says. "It has a central regulatory role, because nothing in your body can go forward without energy. Mitochondria is the missing link between human behavior and human physiology.”
For example, he points out that neurons are “extraordinarily energetically demanding,” and that certain diseases could actually be a mitochondria disease. “All the tissues affected in common diseases also have the highest mitochondria energy demand, and it’s hard to see any anatomical difference between a normal and affected patient, because you can’t see energy,” he says. Wallace makes the case that aging could be chalked up to being “fundamentally the decline of the mitochondria’s ability to produce the energy to power the cells to keep us at optimum health.”
Wallace’s colleague Peter Burke has developed a new technique that makes it possible to analyze the energy of a single mitochondrion. “So now we can understand how subtle changes can have big effects on energy production and physiology,” Wallace says.
Wallace believes that further study could reveal ways to observe and even stop changes in the mitochondria before the obvious symptoms of disease have even begun—and that further research will show that changes in these “energetic genes” will be important in understanding diseases. But he’s concerned that the current scientific paradigm will be slow to embrace it, and thus fund it. He hopes it gets much more research, because he believes it could lead to a whole new generation of neuropsychiatric therapeutics: “This study will lead to a revolution in neuroscience," he says. "Whether the neuroscientists will accept it is another question."