The news is full of terms like superbug, post-antibiotic era, and abbreviations like MRSA. They all refer to various aspects of antibiotic resistance—the ability of bacteria to out-maneuver the drugs that are supposed to kill them and stop an infection.
Now, public health officials are concerned that we could move back into a situation like that of the early 20th century, before antibiotics were discovered. Mental Floss spoke to Dr. Meghan Frost Davis, a veterinarian and associate professor of epidemiology at Johns Hopkins University in Baltimore, Maryland, about some of the potential outcomes of losing antibiotics. “We have generations of recorded history that identify the risks to human society from infectious diseases that we are unable to treat or prevent,” Davis said in 2017.
- Why is antibiotic resistance dangerous?
- Where does antibiotic resistance come from?
- What can you do about antibiotic resistance?
Why is antibiotic resistance dangerous?
If a person becomes ill due to a bacterial infection, they typically see their physician for treatment. But in the years before antibiotics were discovered, people frequently died from scenarios we find difficult to fathom today, including mere cuts or scratches that led to untreatable infections. Ear infections or urinary tract infections could lead to sepsis (bacteria in the blood that can cause organ damage). Arms or legs were surgically removed before an infected wound could lead to death.

When antibiotics were discovered, it's no surprise they were referred to as a “magic bullet” (or Zauberkugel in German, as conceived by medical pioneer Paul Ehrlich). The drugs could wipe out an infection but not harm the host. They allowed people to recover from even the most serious of infections, and heralded a new era in medicine where people no longer feared bacteria.
Davis said the existence of antibiotics themselves has changed how we use medicine. Many medical procedures now rely on antibiotics to treat infections that may result from the intervention. “What is different about a post-antibiotic modern world is that we have established new patterns of behavior and medical norms that rely on the success of antimicrobial treatments,” she said. “Imagine transplant or other major surgeries without the ability to control opportunistic infections with antibiotics. Loss of antibiotics would challenge many of our medical innovations.”
Where does antibiotic resistance come from?
One reason antibiotic resistance is difficult to control is because our antibiotics are derived from natural products. Our first antibiotic, penicillin, came from a common mold. Fungi, bacteria, parasites, and viruses all produce products to protect themselves as they battle each other in their microbial environments. We've taken advantage of the fruits of millions of years' worth of these invisible wars to harness antibiotics for our use. (This is also why we can find antibiotic resistance genes even in ancient bacteria that have never seen modern antibiotic drugs—because we've exploited the chemicals they use to protect themselves).

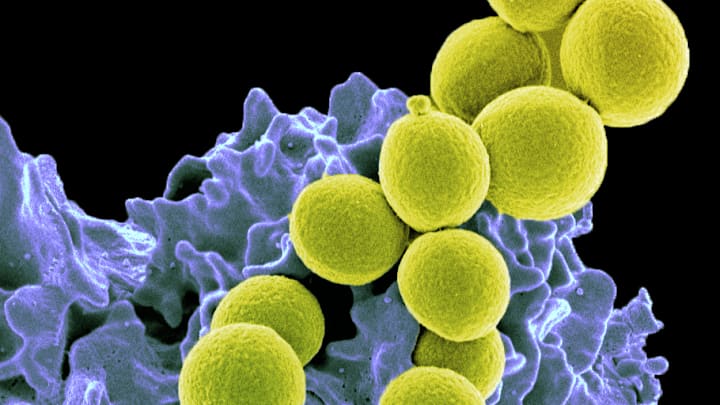
These microbes have evolved ways to evade their enemies—antibiotic resistance genes. Sometimes the products of these genes will render the antibiotic useless by chopping it into pieces or pumping it out of the bacterial cell. Importantly, these resistance genes can be swapped among different bacterial species like playing cards. Sometimes the genes will be useless because the bacteria aren't being exposed to a particular drug, but sometimes they'll be dealt an ace and survive while others die from antibiotic exposure.
And many of these resistance genes are already out there in the bacterial populations. Imagine just one in a million bacterial cells that are growing in a human gut have a resistance gene already in their DNA. When a person takes a dose of antibiotics, all the susceptible bacteria will die off—but that one-in-a-million bacterium that can withstand the antibiotic suddenly has a lot of room to replicate, and the population of bacteria carrying that resistance gene will dramatically increase.
If the person then transfers those resistant gut bacteria to others, resistance can spread as well. This is why it's important to keep control over antibiotic use in all populations—because someone else's use of the drugs can potentially make your own bacteria resistant to antibiotics. This is also why hand washing is important: You can unknowingly pick up new bacteria all the time from other people, animals, or surfaces. Washing your hands will send most of these passenger bacteria down the sink drain, instead of allowing them to live on your body.
What can you do about antibiotic resistance?
You shouldn’t ask for antibiotics from your doctor: If you have a bacterial infection that can be treated by antibiotics, your doctor will prescribe them. Many illnesses are due to viruses (such as the common cold), but antibiotics work only against bacteria. It is useless to take antibiotics for a virus, and doing so will breed resistance in the other bacteria living in your body, which can predispose you or others in your household and community to developing an antibiotic-resistant infection. Remember, those resistant bacteria can linger in your body—in your gut, on your skin, in your mouth, and elsewhere, and can swap resistance genes from the mostly harmless bacteria you live with to the nasty pathogens you may encounter, further spreading resistance in the population.

Antibiotics are also used in animals, including livestock. Purchasing meat that is labeled “raised without antibiotics” will reduce your chance of acquiring antibiotic-resistant bacteria that are generated on the farm and can be spread via meat products.
Davis noted that her clients often requested antibiotics for their pets, even when it was an issue that did not require them. She explained to them why antibiotics were not necessary. “Individuals can partner with their physician and veterinarian to promote good antimicrobial stewardship,” she advised. “Use of antibiotics carries risks, and these risks are related both to side effects and to promotion of resistance. Therefore, decisions to use antibiotics should be treated with caution and deliberation.”
Read More Stories About Health and Medicine:
A version of this story was published in 2017; it has been updated for 2025.