What if you could tweak the genes of a virus to turn its ability to invade cells into a delivery system for eyesight therapy? That’s what researchers at Johns Hopkins School of Medicine say they’ve done by modifying an adenovirus, a type of virus that can infect tissue linings. The cutting edge gene therapy was developed to help those who suffer vision loss from a particular eye disorder—wet age-related macular degeneration (AMD).
Approximately 1.6 million Americans have AMD, the number one cause of vision loss. The disease is characterized by the growth of abnormal blood vessels that leak retinal fluid into the eye and destroy the macula, an area near the retina important for high acuity vision. This gene therapy both reduces fluid buildup and improves vision loss in humans, according to study results published in The Lancet.
The best current treatment for the disease requires injections of antibodies into the retina to suppress vascular endothelial growth factor (VEGF), a protein that is responsible for the growth of blood vessels—which in turn cause leaking fluid. But the problem is that patients must obtain these injections at four- to six-week intervals, or else the disease symptoms return and worsen over time. Peter Campochiaro, a professor of ophthalmology and neuroscience at Johns Hopkins Medicine's Wilmer Eye Institute and one of the authors of the study, explains that during this treatment, if a patient takes too long to get their next injection, the abnormal blood vessel net grows larger and recruits other cells. “That scarring causes permanent decrease in vision,” he tells Mental Floss. So over time, it’s common even for patients in treatment to “end up with less vision.”
His team has been working to make a form of injections that last longer, so patients don’t have to come in as frequently. For phase one of this trial, Campochiaro’s team recruited 19 participants to participate in a 52-week study. He was looking for people “who don’t have great visual potential, but have evidence of the disease process that you can measure in effect,” he says.
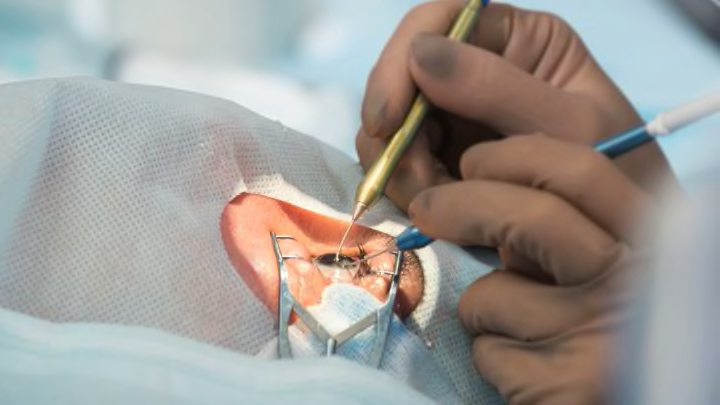
Since viruses are naturally good at getting into cells and depositing their genetic material, the researchers decided to modify a virus to deposit a gene that codes for a protein called sFLT01. sFLT01 blocks the factor that causes the abnormal vessels and fluid production. When the modified virus is injected into the eye, “the viral vector enters cells and deposits the gene, and the gene begins to produce the [sFLT01] protein,” he says. The protein binds to VEGF, preventing it from causing vessel growth and subsequent fluid leakage.
The 19 participants were divided into five different groups and given increasing doses of the viral vector. After determining there was no toxicity at the dose-limit of the first three groups, they proceeded to increase the dosage to its highest level.
Of the 11 participants with symptoms judged to be reversible, six showed “a substantial reduction in the fluid,” and four of those six saw “a pretty dramatic effect.” Those patients had big pockets of fluid in their retinas decrease, Campochiaro says. Better yet, the treatment lasted throughout the yearlong study, though the protein numbers peaked at 26 weeks, and then declined slightly (although not enough to reactivate disease symptoms).
In assessing why five patients saw no reduction in fluid, the scientists discovered those patients had pre-existing antibodies to the virus. They theorize that in these patients, the immune system may have killed the viral vector before it could deposit the genes, though they will have to do more research to prove this. This could be a problem in using this particular virus—a carrier virus called AAV2—since some 60 percent of patients tend to have these antibodies.
A possible solution might be to give resistant patients a surgical injection instead. During this procedure, scientists could take out the vitreous—a gel-like substance that gives your eye its round shape—and inject the vector surgically under the retina instead. While patients might prefer not to have surgery, “our data suggests that it doesn’t matter if there’s pre-existing antibodies [with this method],” he says.
Alternately, other viral vectors have proven to be more effective than AAV2, including a variation on the virus, AAV8, which provides better infections of the virus into the cell. Even more promising, the researchers recently finished a four-year study on a lentiviral vector (a totally different group of viruses) “that take [the genes] into the nucleus of the cell and inserts the gene right into the chromosomes,” Campochiaro explains.
His next steps will be to retest the treatment with a longer study period to identify just how long-lasting the effects are, as well as to test higher doses of the viral vector.
But right now, he is just excited that the gene therapy works. “We injected this gene, the gene is producing a protein, and you can measure that protein in the eye over time,” he says.